 Routine Immunization (RI) is a nation's strategic investment in its future. India's routine immunization program is dynamic and over the years has evolved to address the changing public health needs of the country.
Routine Immunization (RI) is a nation's strategic investment in its future. India's routine immunization program is dynamic and over the years has evolved to address the changing public health needs of the country.
Tremendous gains have been made in immunization coverage in a country where challenges reflect accessibility, acceptability and availability issues.
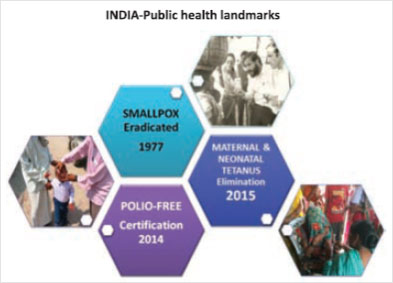
With the success of Small Pox eradication, the Immunization programme was implemented in more organized manner as Expanded Programme of Immunization (EPI) in 1978 targeting under 5 year children only in Urban areas. In 1985 Immunization programme expanded as Universal Immunization Programme ( UIP) which focus under 1 year children, expansion of cold chain etc. The program reached every corner of the country in 1990 and now the program has become an integral part of India's public health infrastructure.
The last five year has seen a dramatic change in the landscape of routine immunization with new vaccines being introduced, the vaccination schedule for Measles and JE changed to 2 dose schedule, open vial policy implemented, strengthening of AEFI system etc. Implementation has been strengthened with capacity building of personnel as well as improvement in service delivery.
| Name of Vaccine | Diseases Prevented |
|---|---|
| Vaccines currently in use in UIP | |
| BCG Vaccine | Tuberculosis |
| DPT Vaccine | Diphtheria, Pertussis (Whooping Cough) and Tetanus |
| Hepatitis B Vaccine | Hepatitis - B |
| Japanese Encephalitis Vaccine | Japanese Encephalitis |
| Measles Vaccine | Measles |
| Oral Polio Vaccine (OPV) | Polio |
| Pentavalent Vaccine | Diphtheria, Pertussis, Tetanus, Hepatitis B, Haemophilus influenzae B Meningitis and Pneumonia |
| Tetanus Toxoid Vaccine | Maternal and Neonatal Tetanus |
| Inactivated Polio Vaccine (IPV) | Polio |
| Rota Virus Vaccine (RVV) | Rota Viral Diarrhoea |
| Newer vaccines to be introduced into the UIP | |
| Pneumococcal Conjugate Vaccine (PCV) | Pneumonia |
| 1978 | Expanded Programme of imunization BCG, DPT, OPV, Typhoid (urban areas) |
| 1983 | TT vaccine for pregnant women |
| 1985 | Universal Immunization Programme - measles added, typhoid removed, Focus on children less than 1yr of age |
| 1990 | Vitamin-A supplementation |
| 1995 | Polio National Immunization Days |
| 1997 | VVM introduced on vaccines in UIP |
| 2002 | Hep B introduced as pilot in 33 districts & cities of 10 states |
| 2005 | National Rural Health Mission Launched Auto Disable (AD) Syringes introduced into UIP |
| 2006 | JE vaccine introduced after campaigns in endemic districts |
| 2007-8 | Hep B expanded to all districts in 10 states & schedule revised to 4 doses from 3 doses |
| 2010 | Measles 2nd dose introduced in RI and MCUP (14 states) |
| 2011 | Hepatitis B universalized and Haemophilus influenza type b introduced as pentavalent in 2 states Open Vial Polisy for vaccines in UIP |
| 2013 | Pentavalent expanded to 9 states Second dose of JE vaccine |
| 2014 | India and South East Asia Reagion certified POLIO-FREE |
| 2015 | India validated for Maternal and Neonatal Tetanus elimination Pentavalent expanded to all tates IPV Introduced New vaccines introduction announced- Rotavirus, Pneumococcal and Measles / Rubella |
| 2016 | Rotavirus Vaccine introduced in 4 states in Phase 1 |
In 1985 the program was changed to Universal Immunization Programme (UIP) and Measles vaccine was added in the same year.
The following are the eight targeted vaccine preventable diseases along with their symptoms, mode of spread and methods of prevention.
2.1.1 How to recognize the Disease?
a) An ill child with a history of contact with a suspected or confirmed case of pulmonary tuberculosis.
b) An ill child with one of the following: Weight loss, cough and wheeze, which does not respond to antibiotic therapy for acute respiratory infection.
2.1.2 How is it spread?
TB is spread when individuals come in contact with cough or sneeze droplets of infected pulmonary tuberculosis individuals. A variety of tuberculosis called Bovine tuberculosis occurs due to consumption of raw cattle milk without boiling.
2.1.3 How is the disease prevented?
Vaccination with Bacillus Calmette-Guerin (BCG) as per the schedule will prevent serious forms of childhood tuberculosis.

Polio is a viral infection that affects the nervous system and can cause severe illness, paralysis, and even death. Due to intensive immunization campaigns, there has been a very significant decline of polio cases in the country since 1999.
2.2.1 How to recognize the disease?
History of sudden onset of weakness and paralysis of the leg(s), and / or arm(s) and/or trunk and history that paralysis was not present at birth or associated with serious injury or mental retardation.
2.2.2 How is it spread?
Polio is transmitted by contact with fecal matter, usually as a result of poor hygiene, or indirectly through contaminated water, milk, or food. More than 50 percent of all cases involve children less than three years of age.
2.2.3 How is the disease prevented?
Immunization with the Oral Polio Vaccine is the only way to effectively prevent infection. Oral Polio Vaccine (OPV) should be routinely administered as per the immunization schedule and during Supplementary Immunization Activities (NID and SNID) till 5 years of age.

Diphtheria is caused by bacteria (Coryne bacterium diphtherae). Diphtheria is an infectious disease that commonly infects the tonsils and pharynx, forming a membrane that can lead to obstructed breathing and death.
2.3.1 How to recognize the disease? Sore throat with gray patch or patches in the throat.
2.3.2 How is it spread?
The bacteria causing diphtheria inhabit the mouth, nose and throat of an infected person. It spreads from person to person by coughing and sneezing.
2.3.3 How is the disease prevented?
The most effective method of prevention is immunization with DPT vaccine in early childhood. Unless immunized, children till 14 ears of age are susceptible to repeat diphtheria infections. DPT vaccine should be given as per the immunization schedule.
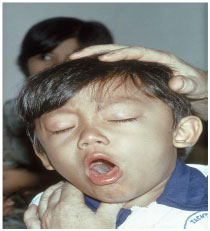
Pertussis, commonly known as whooping cough, is caused by bacteria (Bordetella pertussis). Pertussis is a highly contagious bacterial disease, involving the respiratory tract. It is characterized by repeated cough that may lead to aspiration and possible death, in a few cases.
2.4.1 How to recognize the disease?
A history of repeated and violent coughing, with any one of the following: cough persisting for two or more weeks, fits of coughing, cough followed by vomiting, typical whoop in older infants.
2.4.2 How is it spread?
Pertussis bacteria live in the mouth and nose of the patient and are spread easily through the air, usually from coughing or sneezing.
2.4.3 How is the disease prevented?
DPT vaccine given according to the immunization schedule will prevent Pertussis. Half ofall deaths due to Pertussis are in children less than 12 months.

Tetanus is caused by bacteria (Clostridium tetani). People of all ages can become infected with tetanus.
2.5.1 How to recognize the disease?
Neonatal Tetanus presents with a history of normal suck and cry during the first two days of life, onset of illness between 3 and 28 days of life, inability to suck followed by stiffness of neck and body and/or jerking of muscles.
2.5.2 How is it spread?
Tetanus is present in dirt, intestines and faeces of animals. It enters the body through cuts, punctures or other wounds/infections (like ear infection) and occurs when bacteria come in contact with broken skin or injuries, and also unclean cutting and dressing of the umbilical cord. Neonatal Tetanus (NNT) affects newborn babies that lead to death, if not treated. It generally occurs during the first few days of life, when a woman delivers in unsanitary conditions.
2.5.3 How is the disease prevented?
Immunizing pregnant women and children with TT/DT/DPT as per the immunization schedule is an effective method of preventing both neonatal as well as tetanus in other age groups.
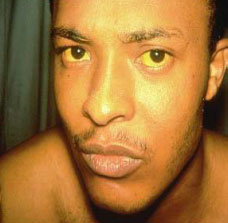
Hepatitis B is a highly infectious viral disease (40-100 times more infectious than HIV) and is the leading cause of jaundice, fulminant liver disease, cirrhosis and liver cancer.
2.6.1 How to recognize the disease?
Clinical signs and symptoms include fever, headache, nausea, vomiting, jaundice (yellowish eyes) and light or gray stools. Final confirmation is done by laboratory tests.
2.6.2 How is it spread?
The disease spreads through contact with infected blood or body fluids. It can be acquired during childbirth, through unprotected sex, use of unsterilized needles and sharing of toothbrushes or razors.
2.6.3 How is the disease prevented?
By immunizing children, we can prevent infection and its complications. Hepatitis B vaccine is given along with DPT at 6, 10, and 14 weeks of age. For institutional deliveries, if first dose has to be given at birth followed by two more doses at 6 weeks and 14 weeks.

Measles is a highly infectious illness caused by a virus that can be found in the nose, mouth or throat of an infected person. Infection is characterized by fever, cough and spreading rash that may lead to death due to secondary infections like diarrhea and pneumonia.
2.7.1 How to recognize the disease?
A history of fever with rash with cough or running nose or red eyes.
2.7.2 How is it spread?
The virus is transmitted through the air by respiratory droplets expelled by infected individuals during coughing and sneezing.
2.7.3 How is the disease prevented?
The measles vaccine is effective in preventing measles and should be given according to the immunization schedule.
Japanese encephalitis (JE) is caused by a virus. It is one of the most deadly forms of viral encephalitis in India. It is prevalent in certain geographical areas in some of the states.
2.8.1 How is it spread?
JE is spread by mosquitoes. The virus normally infects birds and domestic animals, especially pigs. Children get the disease when bitten by mosquito that has bitten an infected animal.
2.8.2 How is the disease prevented?
Immunization is the single most important measure to control Japanese Encephalitis. Separate guidelines will be issued for endemic districts where the JE vaccine will be part of the routine immunization schedule.
National Immunization Schedule
| Sl. No. | Vaccine | Protection | Number of Doses | Vaccination Schedule |
|---|---|---|---|---|
| 1. | BCG((Bacillus calmette Guerin) | Childhood Tuberculosis | 1 | At birth(upto 1 year if not given earlier) |
| 2. | Pentavalent[Diphtheria,Pertussis,Tetanaus(DPT),Hepatitis B and Haemophilus influenza b(Hib) | Diphtheria,Pertussis,Tetanus,Hepatitis B,Haemophilus influenza type B associated Pneumonia and Meningitis | 3 | Three dosage at 6,10 &14 weeks |
| 3. | DPT(Diphtheria,Pertussis and Tetanus Toxoid) | Diphtheria,Pertussis and Tetanus | 2 | Two booster doses at 16-24 month and 5 year of age. Three primary doses at 6,10 & 14 week are part of Pentravalent vaccine |
| 4. | Hepatitis B | Hepatitis B | 1 | Birth does for institutional deliveries with 24 hour. Three primary doses at 6,10 & 14 week are part of pentravalent vaccine |
| 5. | OPV(Oral Polio Vaccine) | Polio | 5 | Birth does for institutional deliveries. Three primary doses at 6,10 & 14 week and one booster dose at 16-24 month of age Given orally |
| 6. | IPV(Inactivated Polio vaccine) | Polio | 1 | One does at 14 weeks, along with OPV3, Injectable dose given |
| 7. | Japanese Encephalitis | Japanese Encephalitis | 2 | 9 to 12 months of age and 2nd does at 16-24 months |
| 8. | Measles | Measles | 2 | 9 to 12 months of age and 2nd does at 16-24 months |
| 9. | Vitamin A | Night Blindness | 9 | -1st does at 9th months -2nd does at 18th months -3rd to 9th does given at 6 monthly interval upto 5 years. |
| 10. | Rota Virus | Rotavirus diarrhoea | 3 | Three doses at 6,10 & 14 week. Given orally |
| 11. | TT (Tetanus Toxoid) | Tetanus | 23 | -10 years and 16 years of age-For pregnant women two doses given(one does if previously vaccinated within 3 years) |
$ At present in six states- Assam, Bihar, Gujarat, M.P, Punjab and U.P, and in process of expansion
# In endemic districts
* Phased introduction, at present in Andhra Pradesh, Haryana, Himachal pradesh and Orissa from 2016
| Age | Immunization Schedule |
|---|---|
| At birth | BCG, OPV (0 dose), hepatitis B (birth dose) |
| 6 weeks (1 ½ months ) | OPV-1, pentavalent-1, Rota Virus Vaccine -1 |
| 10 weeks (2 ½ months ) | OPV-2, pentavalent -2, RVV -2 |
| 14 weeks (3 ½ months ) | OPV-3, pentavalent -3, RVV-3 & IPV |
| 9-12 months | Measles first dose, JE- 1, Vit. A |
| 16–24 months | DPT-booster first dose, measles second dose, OPV booster dose , JE second dose |
| 5–6 years | DPT-booster second dose |
| 10 years | TT first booster dose |
| 16 years | TT second booster dose |

As a startegies endeavour the ministry of health and family wealfare(MoHFW), Government of india,launched Misson Indradhanush in december 2014
The mission focueses om interventions to improve full immunization coverage for children in india from 65% in 2014 to atleast 90% over next five years through special cathch up drives.
Four states -Bihar, Madhya Pradesh ,Rajasthan and, Uttar Pradesh- account for 82 of the 201 high focus districts and nearly 25% of the unvaccinated or partially vacvinated Children.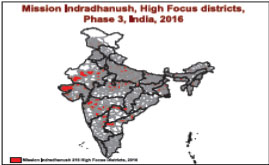
Based on prioritization, the country has been categorazied in to high, medium and low focus districts. Phase I of mission indhradhanush targeted 201 high-focus districts,with four rounds of activity between april and july 2015.Phase 2 targeted 352 districts (73 districts repeated from Phase 1) with four rounds of activity between october 2015 and January 2016.
During these two phases of mission indradhanush more than 3.7 million children were fully immunized and about 3.7 million pregnant women.Phase iii of MI in 2016 will reach out to 2016 high focus districts across 27 states/union territories
The "cold chain" refers to the people, equipment, and procedures designed to maintain appropriate temperatures for vaccines from the time they leave the manufacturer, through transportation and storage, until the point of use. Health workers are responsible to maintain the temperature of vaccines at the peripheral level. If a vaccine is exposed to too much heat, light or cold, it can be damaged and lose its potency or effectiveness. If that happens, all the effort to give the vaccine to the child is lost.
Vaccines lose their potency due to exposure to
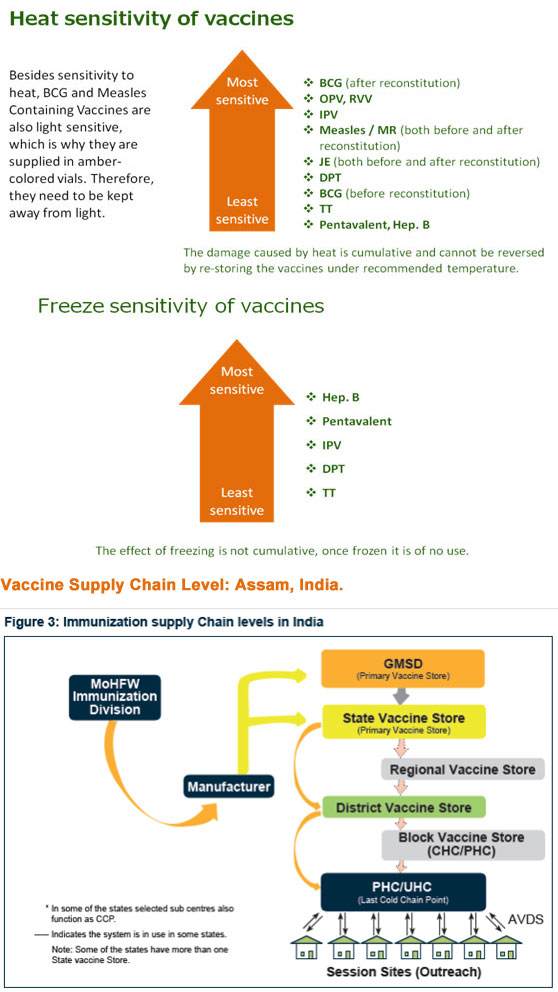
Present Status of Vaccine Stores in Assam
| Vaccine Store | Numbers |
|---|---|
| GMSD | 4 |
| State Vaccine stores | 1 |
| Regional Vaccine stores | 5 |
| District Vaccine stores | 27 |
| CHC / PHC / UHC / Other Hospitals / Last Cold Chain Point | 816 |
| Total CCPs in Assam | 849 |
The public use of vaccines in India has had an impressive impact on the morbidity and mortality of VPDs. various studies and surveys over the years have quantified these changes. The info graphic below demonstrate the successes but also reminds us of the need to increase our efforts to further strengthen and sustain RI.
The coverage Evaluation Survey 2009 identified the reasons for not accessing immunization services as cited by community. A majority had demand-side issues, e.g. did not feel the need of vaccination; did not know about vaccines or where to go for vaccination; time not convenient; fear of side-effects; or did not have time.
Recent data from house-to-house RI Monitoring in UP also highlighted lack of awareness and fear of AEFIs as major reasons for missed children as shown in fig.9.3.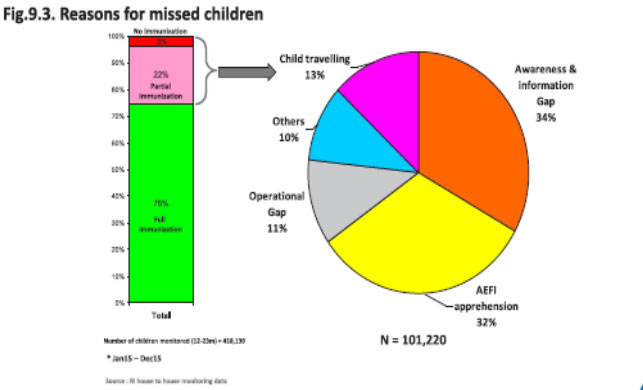
A correctly and completely filled infant immunization card contains mother's and child's name, date of birth, complete address and immunization status. The immunization card is important for the following reasons :
Reminds the parents which vaccines have been given and which vaccines are due
Reminds the parents which vaccines have been given and which vaccines are due.
Universal Immunization Programme
At present all infants and children upto the age of 16yrs of the State are getting vaccination against the vaccine preventable diseases. In the beginning, vaccination was done against the diseases of poliomyelitis, Tuberculosis, Diphtheria, Pertusis (Whooping Cough), Tetanus and Typhoid. Moreover, 2 doses of TT were given to Pregnant Women.
Thereafter, the Govt. of India introduced the Programme of vaccination under" Universal Immunization Programme" since 1985.
| Age | Immunization Schedule |
|---|---|
| At birth | BCG, OPV (0 dose), Hepatitis B (birth dose) |
| 6 weeks (1 ½ months ) | OPV-1, Pentavalent-1 |
| 10 weeks (2 ½ months ) | OPV-2, Pentavalent -2 |
| 14 weeks (3 ½ months ) | OPV-3, Pentavalent -3 & IPV |
| 9 months | Measles first dose, JE- 1, Vit. A |
| 16–24 months | DPT-booster first dose, measles second dose, OPV booster dose , JE second dose |
| 5–6 years | DPT-booster second dose |
| 10 years | TT first booster dose |
| 16 years | TT second booster dose |
Circulars and Guidelines on Immunization:
Guideline & Hand Books:
Registers & Formats:
Fact Sheets
The achievement of last Five years are as follows :
| Full Immunization Coverage: | 2011 - 2012 | 77.37 % |
| For infant | 2012 – 2013 | 83.80% |
| 2013 – 2014 | 87.57% | |
| 2014 – 2015 | 86.15% | |
| 2015 – 2016 | 88.18% |
For strengthening Routine Immunization Mission Indradhanush Strategy to cover Drop and Left out strategy was introduced from 7th April'2015 in 8 districts for Phase –I and continue in moderate 18 districts from 7th Oct' 2015 for phase _II and again completed 4 rounds in 12 districts from 7th April'2016 for Phase -III.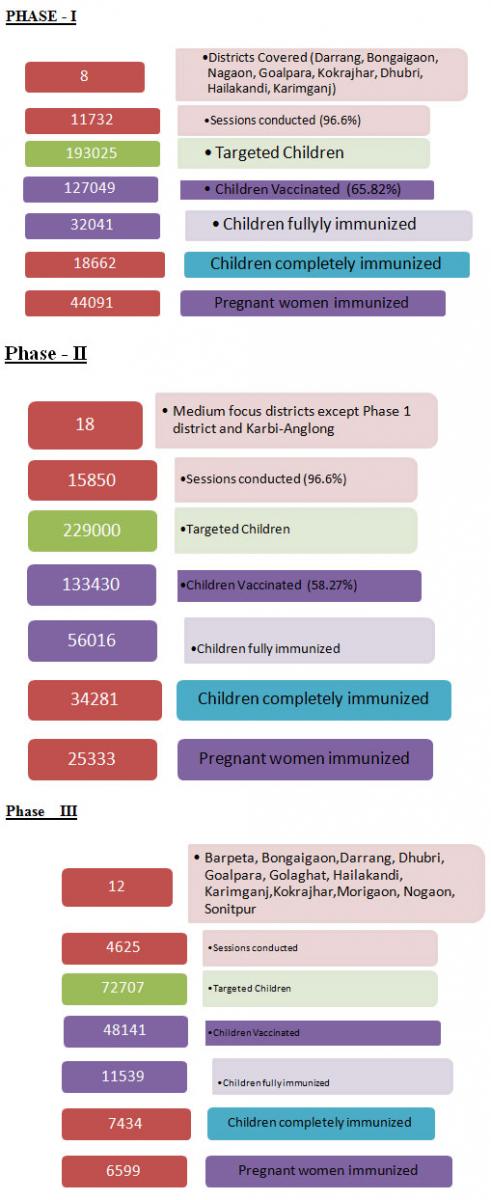
Starting from 2006 -07, we have completed children Vaccination campaign of age group 1 -15 yrs in all the 27 districts of Assam and vaccinated more that 87 lakhs of children . For the age group 0 – 1 yrs and 1 – 2 yrs the routine JE Vaccine is being carried out in all the districts of Assam.
During 2013 -14 , we have completed Adult JE Vaccination Campaign of age group 15 – 65 yrs in Lakhimpur, Dibrugarh, Sivasagar, Tinsukia, Jorhat, Dhemaji, Goalghat, Kamrup®, Sonapur Block of Kamrup (M). And during 2015 – 2016 Adult JE Vaccination Campaign was implemented in Darrang, Nagaon, Sonitpur, Barpeta, Udalguri . In above 13 district about 64 lakhs adult beneficiaries were vaccinated.
During current year 2016 -17 it is proposed for Adult JE Vaccination in Cachar (Case – 9, Death-0) , Morigoan (Case – 9, Death-2), Nalbari (Case – 10, Death-5) , Bongaigaon (Case – 5, Death-1) and Block wise target beneficiaries (total 23 lakhs) which is to be vaccinated is already communicate to GOI for release for Vaccine and syringes and also for related fund through ROP (C.1.u 2016 -17).
Thereafter, PPI (Pulse Polio Immunization) was introduced in 1995 and yearly two rounds of Pulse Polio Immunization are launching till now through NID & IPPI progamme against Polio Myelitis. Now, India is not having Polio Myelitis case since 13th Jan'2011 till to-day the 6/08/2013 and WHO has declared "Polio – Free - India" on March'2014.
Major Achievement of the Programme
Immunization performance report of assam
| Year | Antigen | Target | Achievement | % | ||||
|---|---|---|---|---|---|---|---|---|
| 2012-2013 | DPT 3 | 705011 | 615043 | 87.24 | ||||
| OPV 3 | 705011 | 609159 | 86.40 | |||||
| BCG | 705011 | 670558 | 95.11 | |||||
| Measles | 705011 | 607229 | 86.13 | |||||
| Fully Imm | 705011 | 590806 | 83.80 | |||||
| TT(PW) | 815032 | 647035 | 79.39 | |||||
| HEP- B | ||||||||
| HEP-B1 | 705011 | 622236 | 88.26 | |||||
| HEP-B2 | 705011 | 601815 | 85.36 | |||||
| HEP-B3 | 705011 | 542628 | 76.97 | |||||
| JE | 345460 | 202929 | 58.74 | |||||
| Measles 2nd Dose | 642680 | 131414 | 20.45 | |||||
| 2013-2014 | DPT 3 | 680900 | 625389 | 91.85 | ||||
| OPV 3 | 680900 | 617381 | 90.67 | |||||
| BCG | 680900 | 609622 | 89.53 | |||||
| Measles | 680900 | 611964 | 89.88 | |||||
| Fully Imm | 680900 | 596264 | 87.57 | |||||
| TT(PW) | 776919 | 677865 | 87.25 | |||||
| HEP- B | ||||||||
| HEP-B1 | 680900 | 601978 | 88.41 | |||||
| HEP-B2 | 680900 | 590654 | 86.75 | |||||
| HEP-B3 | 680900 | 573563 | 84.24 | |||||
| JE-1st Dose | 305420 | 230169 | 75.36 | |||||
| JE-2nd Dose | 282769 | 170735 | 60.38 | |||||
| Measles 2nd Dose | 615969 | 401704 | 65.21 | |||||
| 2014-2015 | DPT 3 | 668181 | 606723 | 90.80 | ||||
| OPV 3 | 668181 | 560613 | 83.90 | |||||
| BCG | 668181 | 674420 | 100.93 | |||||
| Measles | 668181 | 586879 | 87.83 | |||||
| 2014-2015 | Fully Imm | 668181 | 575634 | 86.15 | ||||
| TT(PW) | 777777 | 661114 | 85.00 | |||||
| HEP- B | ||||||||
| HEP-B1 | 668181 | 564521 | 84.49 | |||||
| HEP-B2 | 668181 | 595478 | 89.12 | |||||
| HEP-B3 | 668181 | 588436 | 88.07 | |||||
| JE-1st Dose | 394553 | 283922 | 71.96 | |||||
| JE-2nd Dose | 358467 | 196526 | 54.82 | |||||
| Measles 2nd Dose | 629426 | 437998 | 69.59 | |||||
| 2015-2016 | DPT 3 | 680528 | 99890 | 14.68 | ||||
| OPV 3 | 680528 | 599265 | 88.06 | |||||
| BCG | 680528 | 636518 | 93.53 | |||||
| Penta -1 | 680528 | 619487 | 91.03 | |||||
| Penta-2 | 680528 | 588635 | 86.50 | |||||
| Penta-3 | 680528 | 525177 | 77.17 | |||||
| Measles | 680528 | 612154 | 89.95 | |||||
| Fully Imm | 680528 | 600067 | 88.18 | |||||
| TT(PW) | 791318 | 656817 | 83.00 | |||||
| HEP- B | ||||||||
| HEP-B1 | 680528 | 19856 | 2.92 | |||||
| HEP-B2 | 680528 | 49997 | 7.35 | |||||
| HEP-B3 | 680528 | 98611 | 14.49 | |||||
| JE-1st Dose | 637341 | 448432 | 70.36 | |||||
| JE-2nd Dose | 602927 | 365425 | 60.61 | |||||
| Measles 2nd Dose | 643781 | 512784 | 79.65 | |||||
| 2016-2017( April'16 to May'2016) | DPT 3 | 680220 | 530 | 0.08 | ||||
| OPV 3 | 680220 | 93634 | 13.77 | |||||
| BCG | 680220 | 96616 | 14.20 | |||||
| Penta -1 | 680220 | 104341 | 15.34 | |||||
| Penta-2 | 680220 | 102276 | 15.04 | |||||
| 2016-2017( April'16 to May'2016) | Penta-3 | 680220 | 94366 | 13.87 | ||||
| Measles | 680220 | 84913 | 12.48 | |||||
| Fully Imm | 680220 | 83563 | 12.28 | |||||
| TT(PW) | 756438 | 106263 | 14.05 | |||||
| HEP- B | ||||||||
| HEP-B1 | 680220 | 3227 | 0.47 | |||||
| HEP-B2 | 680220 | 616 | 0.09 | |||||
| HEP-B3 | 680220 | 2182 | 0.32 | |||||
| JE-1st Dose | 680220 | 69296 | 10.19 | |||||
| JE-2nd Dose | 643489 | 57231 | 8.89 | |||||
| Measles 2nd Dose | 643489 | 84284 | 13.10 | |||||
| Year | Name of the District | Target | Achievement | % |
|---|---|---|---|---|
| Children - (1-15 Yrs) | ||||
| 2006-07 | Dibrugarh | 409611 | 370653 | 90.49 |
| Sivasagar | 386228 | 264591 | 68.51 | |
| Golaghat | 196304 | 135924 | 69.24 | |
| Jorhat | 206095 | 186118 | 90.31 | |
| 1198238 | 957286 | 79.89 | ||
| 2008-09 | Tinsukia | 419964 | 387608 | 92.30 |
| Dhemaji | 212236 | 187772 | 88.47 | |
| 632200 | 575380 | 91.01 | ||
| 2009-10 | Lakhimpur | 380710 | 315731 | 82.93 |
| Sonitpur | 650156 | 431387 | 66.35 | |
| Kamrup(R) | 501318 | 351040 | 70.02 | |
| 1532184 | 1098158 | 71.67 | ||
| 2010-11 | Nagaon | 859192 | 795429 | 92.58 |
| Sivasagar | 437427 | 369659 | 84.51 | |
| Dibrugarh | 431690 | 400989 | 92.89 | |
| Udalguri | 281792 | 199878 | 70.93 | |
| 2010101 | 1765955 | 87.85 | ||
| 2013-14 | Barpeta | 558753 | 420151 | 75.19 |
| Darrang | 304764 | 273591 | 89.77 | |
| Goalpara | 331584 | 257720 | 77.72 | |
| 1195101 | 951462 | 79.61 | ||
| 2014 -15 | Morigaon | 331997 | 200574 | 60.41 |
| Nalbari | 272601 | 203915 | 74.80 | |
| Sonapur Block of Kamrup(M) | 65442 | 41193 | 62.95 | |
| 670040 | 445682 | 66.52 | ||
| 2015 -16 | Bongaigaon | 256267 | 211570 | 82.56 |
| Baksa | 331365 | 226423 | 68.33 | |
| Cachar | 608414 | 511484 | 84.07 | |
| Chirang | 164451 | 74943 | 45.57 | |
| Dhubri | 676405 | 548344 | 81.07 | |
| Dima Hasao | 73357 | 60128 | 81.97 | |
| Hailakandi | 231824 | 197121 | 85.03 | |
| Kamrup (Metro) | 374661 | 202787 | 54.13 | |
| Karimganj | 420825 | 381653 | 90.69 | |
| Karbi-Anglong | 336650 | 273568 | 81.26 | |
| Kokrajhar | 307621 | 171263 | 55.67 | |
| 3781840 | 2859284 | 75.61 | ||
| 2013-14 | Adult - (15-65 Yrs) | |||
| Lakhimpur | 581331 | 482668 | 83.03 | |
| Dibrugarh | 734295 | 683138 | 93.03 | |
| Sivasagar | 197886 | 135131 | 68.29 | |
| Tinsukia | 731925 | 467697 | 63.90 | |
| Jorhat | 600192 | 538667 | 89.75 | |
| Dhemaji | 386800 | 303038 | 78.34 | |
| Golaghat | 585371 | 473485 | 80.89 | |
| Kamrup-Sonapur | 104030 | 74264 | 71.39 | |
| Kamrup® | 845217 | 561455 | 66.43 | |
| 4767047 | 3719543 | 78.03 | ||
| 2015-16 | Darrang | 479006 | 400814 | 83.68 |
| Nagaon | 1538946 | 710330 | 46.16 | |
| Sonitpur | 1051593 | 748133 | 71.14 | |
| 3069545 | 1859277 | 60.57 | ||
| Barpeta | 920160 | 601533 | 65.37 | |
| Udalguri | 448164 | 239710 | 53.49 | |
| 1368324 | 841243 | 61.48 | ||
| Sl. No. | Year | Target (Estimated) | Achivment | Percentage | Wild Poliovirus Status |
|---|---|---|---|---|---|
| 1. | 2011-12 Feb.'12 (NID 1ST Round) | 4637240 | 4624188 | 99.72 % | NIL |
| 2011-12 April.'12 (NID 2nd Round) | 4631872 | 4607834 | 99.48 % | NIL | |
| 2. | 2012-13 Jan'13 (1st Round) | 4755475 | 4616095 | 97.00 % | NIL |
| 2012-13 Feb'13 (2nd Round) | 4755475 | 4633736 | 97.44 % | NIL | |
| 3. | 2013- 14 19th Jan'14 ( NID 1st Round) | 4787494 | 4678302 | 97.72% | NIL |
| 2013 – 14 Feb'14 ( NID 2nd Round) | 4790780 | 4689569 | 97.89% | NIL | |
| 4. | 2014-15 18th Jan'2015 ( NID 1st Round) | 4725542 | 4676315 | 98.96% | Nil |
| 2014-15, 22nd Feb'2015 ( NID 2nd Round) | 4725542 | 4712623 | 99.73% | NIL | |
| 5. | 2015-16 24th Jan'2016 ( NID 1st Round) | 4725543 | 4730917 | 100.11 | Nil |
| 2015-16, 21st Feb'2016 ( NID 2nd Round) | 4808406 | 4700750 | 97.76 | Nil |
| Title | Size | Detail |
|---|---|---|
| Immunization Card | 1.85 MB | |
| Current UIP Schedule | 92.31 KB | |
| Routine Immunization Details - for 4th August Meting | 4.13 MB | |
| Job Responsibilities of Staff in Immunization Program | 521.45 KB |
